Prioritization and Queue Discipline
In the previous post, I finished with the discussion regarding the prioritization and queue discipline and argued that the service needs to be provided equitably, equally and fairly.
Equitable service delivery requires giving a higher priority for people who has a higher need for service. Person who is unable to walk should get the hip surgery earlier than a person who is able to walk. The quality of life of the person who can't walk has deteriorated more than the one who can walk. In order to identify who has the most need, a prioritization method is required. The prioritization method needs to consider several variables, such as current status of illness, speed of disease progression, the impact of the disease, and social factors. It would be ideal to find tools that can provide an objective assessment of the variable(s) but it is not likely to find one for all possible problems. Here are some examples.
Of the two people who has Parkinson's, the person whose disease progresses faster can have the deep brain stimulator earlier.
|
|
Impact of the disease
(life or limb)
|
A person who has cancer should receive services earlier because the delay could result in loss of life. A person who has malignant melanoma should receive services earlier than a person with spinocellular carcinoma because maligant melanoma has a higher potential for spread.
|
Social factors
|
The weights of these factors in determining priority might be different but, at the end, a priority must be given to each individual. Ideally, individuals should be able to compare their priority against the others' on the waitlist. Having transparency of the waitlists satisfies the need for fairness.
Equal access to services means a person with a particular need should access the services in the same time frame across service providers. For example, if there are five outpatient clinics of a hospital (or five physicians in the practice), all persons who have the same priority should have same average wait time for the services. This ensures that other conditions, such as location, culture, race, language, income, employment, etc. are not factors in accessing the services.
Fairness means you access the services based on your priority and the time that you waited must count for something. You would not wait endlessly for a service and pushed constantly to the end of the queue because people with more urgent conditions arrive. However, this may happen in waitlist management for the following reasons.
- Either more urgent cases come (who has the same priority but due to factors that are not captured in the priority) and bump the cases who are on the list to the end of the list.
- People who are waiting cannot get their turn when called and they continue waiting. For example, for surgical waitlist, when the patient was given a surgery date and they can't accept it because they are recovering from another ailment, or they have planned to go somewhere, etc.
- There are external forces to encourage selecting patients who waited less. When there is performance measure of percent served within their target wait time and it is calculated based on people who received their service, service provider may inclined to provide service to people who are not above their wait time target first in order to ensure their performance is high.
- Lastly, as human brain cannot process data easily, we tend to remember the patients that we have seen recently and tend to engage in discussion with them and provide service to them earlier. People who were waiting for a long time continue to wait.
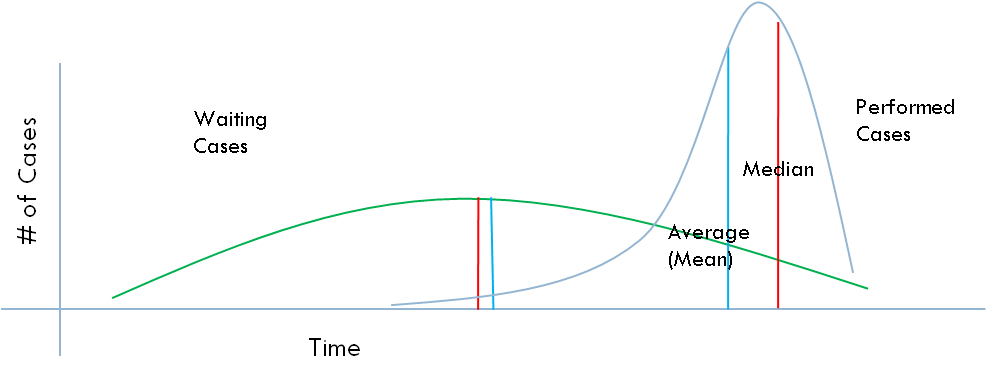
How does the distribution of cases look like against their target, if above factors influence the decision to select patients/customers from the list? For the sake of argument, lets call this First-In- Last-Out (FILO).
People who receive the service receive (above graph performed cases indicating that the patients received their surgery) significantly earlier than the cases waiting during the same time period.
If we randomly select the cases from the waitlist, sometimes we will select a patient that just started waiting and sometimes a patient that has the longest wait time. The distribution will look like a normal distribution. Let's call this random selection (RS)
In this case, eveybody on the waitlist has an equal chance of being picked at any point. The average wait time for performed cases and the waiting cases would be exactly the same (or close).
We get the person who waited the longest from the end of the queue (in-turn). This uses the First-In-First-Out (FIFO) principle.
If we randomly select the cases from the waitlist, sometimes we will select a patient that just started waiting and sometimes a patient that has the longest wait time. The distribution will look like a normal distribution. Let's call this random selection (RS)
In this case, eveybody on the waitlist has an equal chance of being picked at any point. The average wait time for performed cases and the waiting cases would be exactly the same (or close).
We get the person who waited the longest from the end of the queue (in-turn). This uses the First-In-First-Out (FIFO) principle.
In this graph, the wait time for the cases waiting at any time is shorter than the cases that received their service. There may be some cases that receive their services earlier but this is certainly not the norm. I don't know which queue among the above three you would like to be in but I certainly prefer the last one.
Based on this view, the IRMACS at the Simon Fraser University (http://www.irmacs.sfu.ca/) came up with a basic indicator. Let's call it Queue Discipline Ratio. It is simply the division of average wait time for performed (or people who received their service) cases by the average wait time for the waiting cases. Random selection will give you a number around 1. The higher the number the more closer the queue discipline to FIFO.
This is quite easy to implement if we have only one queue without differing priorities. What if we have several priorities, can we actually use this? Next post will cover this. Here is an example.
Blue lines are the cases performed (or received their service) and red lines are the cases still waiting with a particular priority. How can we achieve, and track, queue discipline for this waitlist?
Based on this view, the IRMACS at the Simon Fraser University (http://www.irmacs.sfu.ca/) came up with a basic indicator. Let's call it Queue Discipline Ratio. It is simply the division of average wait time for performed (or people who received their service) cases by the average wait time for the waiting cases. Random selection will give you a number around 1. The higher the number the more closer the queue discipline to FIFO.
This is quite easy to implement if we have only one queue without differing priorities. What if we have several priorities, can we actually use this? Next post will cover this. Here is an example.
Blue lines are the cases performed (or received their service) and red lines are the cases still waiting with a particular priority. How can we achieve, and track, queue discipline for this waitlist?



No comments:
Post a Comment