A lot has been written about how to reduce and eliminate waitlists. This post is not concerned about reducing or eliminating waitlists but understanding your waitlists and how to manage them. The solution alternatives for reducing or eliminating waitlist are political and complex decisions and much has been written about them. Again my focus here is how can we manage the existing waitlist.
Here is what we need to know for effectively managing the waitlist.
Arrivals
Number of people coming on the
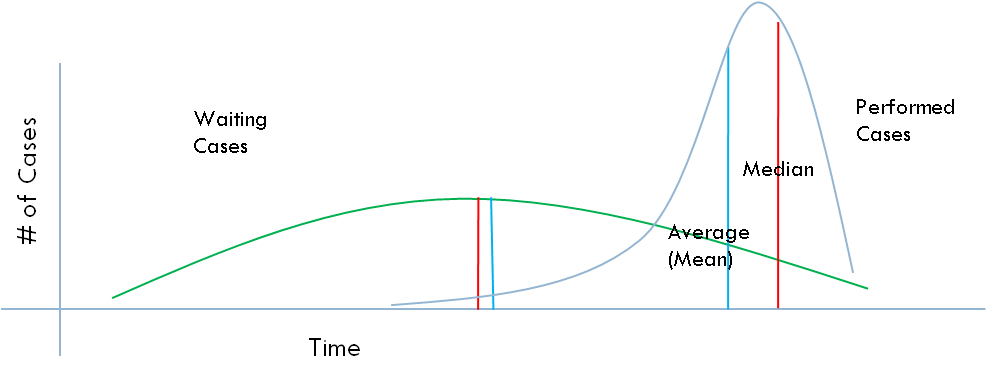
your waitlist presents the load on the waitlist, it is measured by a time period. It is important to know the volume of arrivals, especially if you have control over the resources, you can plan for the supply. The gap between the number of people processed (or removed from the waitlist) versus the number that added on the waitlist indicates the whether your waitlist is growing or shrinking. In surgical waitlists, this is the number of patients booked for surgery; in a physician office this number of referrals or number of people who request an appointment. You wouldn't expect your local grocer to have only one cashier all day every day. You would expect them have more cashiers at peak times. This is why knowing the volume of arrivals and understanding the fluctuations in the number of arrivals is important.
Capacity
Depending on the business, this might be number of people working and existing infrastructure (e.g. number of cubicles, or number of check-out terminals, number of operating rooms, number of examination rooms, number of ultrasound machines). For example, the capacity question in the surgical waitlist may not be the number of surgeons available but number of hospital beds available because the hospital beds might be the determinant of the throughput rather than the surgeons or OR capacity. Knowing the the determinants of the throughput and their impact on the waitlist is critical. The determinant of the throughput will change as the capacity in various part of the flow changes. If you suddenly given 20 hospital beds (or two additional examination rooms) the determinant may become OR time (or available staff). It is important to have a map of all items that determine the capacity on a particular flow, identify the maximums and minimums required based on the arrivals.Capacity planning involves the volume of arrivals, the volume of waitlist that you would like to have and the acceptable perceived wait time.
Queuing theory, advance access and simulations using these are some of the tools to match the waitlist and wait time to the existing capacity. These tools would also help with exploring the possibilities of reorganizing service provision in order to use the existing resources more efficiently. For example, if the service that is provided is a standard one and it doesn't matter who provides the service (e.g. airport check-in) one single queue and first available provider is the most efficient model. But if personal relationship is important or you have other objectives (such as having customers to hang out longer in front of magazines and candy) then having separate lines and allowing customers (patients) to choose their providers might be a better option.
Wait Time
Time between the start and the end of wait identifies how long individuals wait for service. When the wait starts and when it ends may differ depending on the perspective. For example, while the wait starts for the patient when a decision is made, the wait may only start for the provider organization when patient contacted them.
The critical factor in wait time is not the actual wait time but the users' perceived wait time. This determines the satisfaction with the waiting. There are factors affecting the perceived wait time. For example, literature suggests that knowing accurately how long one will wait,
communicating with the system and other waiters during the wait, and keeping
active during the wait reduces the perceived wait. More specifically unoccupied time, reprocess waits, uncertain waits or anxiety during waiting, unexplained and unfair waits, and solo waits seem longer than occupied time, in-process waits, known waits, explained waits, and group waits1,2.Patient tend to value short waiting times and also the possibility of influencing the date/time of the service (e.g. appointment, surgery)3.
Lets consider some examples of reducing perceived wait for a physician office or surgery.
Characteristic
|
Physician Office
|
Surgical Services
|
Knowing expected wait time
|
Estimated time that physician sees you. e.g. You will be seen in 20 minutes.
|
Expected date of surgery (or the expected week that surgery is going to be scheduled).
|
Communicating
|
Talking with the medical office assistant, acknowledgement of your arrival, estimated wait time, and reviewing anything related to your patient file.
|
Updates from the surgical system, meeting with other patients who are waiting for the same surgery (physically or virtually) and possibly tracking and submitting your improvement to the surgical system (see below)
|
Keeping Active
|
Completing a specific or general assessment of your health (e.g. SF-36, Euro-Qol) and receiving a comparison where you were in the past.
|
Getting ready for surgery with exercise regiments (e.g. pulmonary conditioning, diabetes control), physiotherapy support (muscle strength), and education.
|
Patient satisfaction is a function of the difference between the perceptions and expectations. If we can deliver service earlier than patient's expected wait time or deliver service within the perceived wait time, patients are likely to be satisfied.
- We can improve their satisfaction with providing equitable, equal and fair service4,5.
- We can improve their satisfaction by providing information to set reasonable expectations4
- We can improve their satisfaction by involving them in activities, groups and constant communication and not allowing them to have a lonely waiting experience, their perceived wait time would decrease4.
Perceptions with wait time also affects user's perceptions of the service. When individual's are unhappy with their wait, they attributed their unhappiness to the service quality as well
4.
Maximum Length of Waiting Line
From the service point of view, having a wait list (or waiting line) is good. As a manager of the service, you can maximize the use of your resources. You can keep your productivity on a higher level. If you are restaurant operator, you may want to increase your table occupancy rate by keeping a waitlist. However, there needs to be a balance between the length of the waitlist and users perception of an acceptable waitlist. Users of the service should consider getting in line and should not be overwhelmed with the length of the waiting line that they should search for an alternative service or provider.
For emergency or drop-in services queue is generally visible. For elective (or appointment based) health care services, there is no visible queue. However, it is still important
have a sense of the number of people waiting or more importantly number of people
waiting against the capacity. The number of people waiting against capacity is a more valuable indicator, particularly if one wants to keep a certain level of demand for counteract fluctuations in demand, for example one week or one month service equivalent of demand (waitlist). If you are a restaurant operator, may be half-an-hour of demand is all what you can hope for.
Prioritization and Queue Discipline
If you are waiting for your service, you want to be sure that the service is provided equitably, equal and a fair way. What do I mean by equitable? Equitable means that you receive the service based on your needs. For example, one would not expect that a person who is having a heart attack waits as long as the patient who has an ankle sprain. In this case, we expect that the person with higher need goes first. What do I mean by equal? Patients who have the same need should access the same opportunity to services. In other words, all people who are waiting for an x-ray for their sprained ankle should wait the same amount of time. What do I mean by fairness? There needs to be justice in service access. The time that one waited should count for something. It should not be fair for anyone to wait for 24 hours in the emergency because there is constant flow of more urgent patients. At one point, the waited time should enable the individual to become urgent. I will explore the prioritization and queue discipline in the next post.
***************************
1 Lee, W., Lamber, C (2000) Impact of waiting time on evaluation of service quality and customer satisfaction in food service operations, Foodservice Research International, V.12, pp.241-254
2 Sridar, MS. (unknown) Waiting Lines and Customer Satisfaction, downloaed May 1, 2014 from
www.researchgate.net/...Waiting_Lines.../d912f50a3d915e080f.pdf
3 Lofvendahl et al (2005) Waiting for orthopaedic surgery: factors associated with waiting times and patients' opinion, International Journal of Quality in Health Care, V.17, No.2, pp.133-140
4 Davis, M.,Heineke, J (1998) How disconfirmation, perception and actual waiting times impact customer satisfaction, International Journal of Service Industry Management, V.9, No.1, pp.64-73
5 Conner-Spady, B et al (2011) The importance of patient expectations as a determinant of satisfaction with waiting times for hip and knee replacement surgery, Health Policy, V.101, pp.245-252